ACL Reconstruction
Introduction:
* The Anterior Cruciate Ligament is one of the major stabilizing ligaments in the knee. It is a strong rope like structure located in the center of the knee running from the femur to the tibia.
* When this ligament tears, unfortunately it doesn’t heal and often leads to the feeling of instability in the knee.
* ACL reconstruction is a commonly performed surgical procedure and with recent advances in arthroscopic surgery can now be performed with minimal incisions and low complication rates.
Function:
* The ACL is the major stabilizing ligaments in the knee. It prevents the tibia (Shin bone) moving abnormally on the femur (thigh bone). When this abnormal movement occurs it is referred to as instability and the patient is aware of this abnormal movement.
* Often other structures such as the meniscus, the articular cartilage (lining the joint) or other ligaments can also be damaged at the same time as a cruciate injury and these may need to be addressed at the time of surgery.
History of Injury:
- Most injuries are sports related involving a twisting injury to the knee
- It can occur with a sudden change of direction, a direct blow e.g., a tackle, landing awkwardly
- Often there is a popping sound when the ligament ruptures
- Swelling usually occurs within hours
- There is often the feeling of the knee popping out of joints
- It is rare to be able to continue playing sport with the initial injury
Diagnosis:
The diagnosis can often be made on the history alone.
Examination reveals instability of the knee, if adequately relaxed or not too painful.
An MRI (Magnetic Resonance Imaging) can be helpful if there is doubt as well as to look for damage to other structures within the knee.
At times the final diagnosis can only be made under anesthetic or with arthroscopic surgery.
Treatment:
Initial
- Rest
- Ice
- Elevation
- Bandage
* Not everyone needs surgery. Some people can compensate for the injured ligament with strengthening exercises or a brace.
* It is strongly advised to give up sports involving twisting activities, if you have an ACL injury.
* Episodes of instability can cause further damage to important structures within the knee that may result in early arthritis.
Indications for Surgery
* Young patients wishing to maintain an active lifestyle Sports involving twisting activities e.g., soccer, basketball, football
* Giving way with activities of daily living People with dangerous occupations e.g., policemen, firemen, roofers, scaffolders
* It is advisable to have physical therapy prior to surgery to regain motion and strengthen the muscles as much as possible.
Surgery:
Surgical techniques have improved significantly over the last decade, complications are reduced and recovery much quicker than in the past.
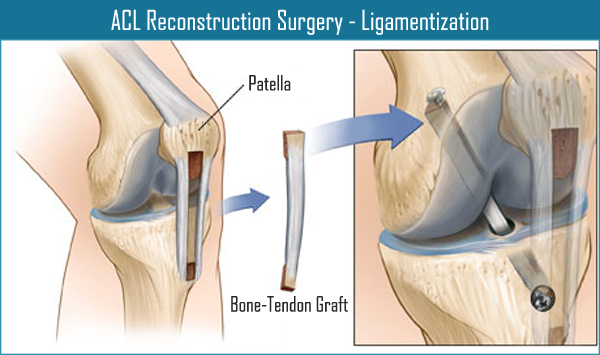
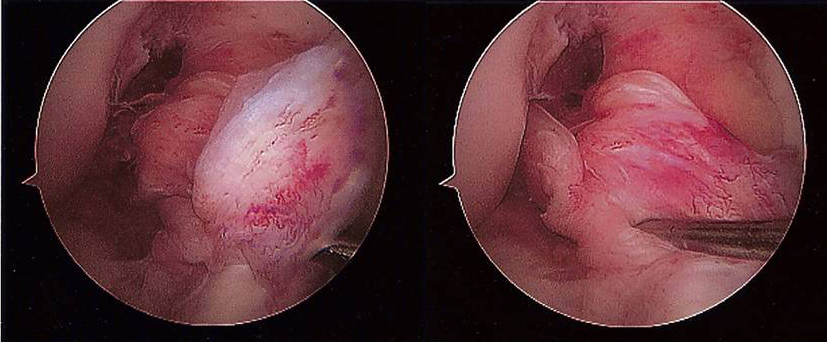
* The surgery is performed arthroscopically. The ruptured ligament is removed and then tunnels (holes) in the bone are drilled to accept the new graft. This graft that replaces your old ACL is taken either from the hamstring tendon or the patella tendon. There are advantages and disadvantages of each with the final decision based on your surgeons preference.
* The graft is prepared to take the form of a new tendon and passed through the drill holes in the bone.
* The new tendon is then fixed into the bone with various devices to hold it into place while the ligament heals into the bone (usually 6 months)
* The rest of the knee can be clearly visualized at the same time and any other damage is dealt with such as meniscal tears.
* The wounds are then closed, often with a drain in place, and a dressing applied.
Post-Operation:
- Surgery is performed as a day surgery or overnight.
- You will have pain medication by tablet or in a IV.
- Any drains will be removed from the knee.
- A splint is sometimes used for comfort.
- You will be seen by a physical therapist who will teach you to use crutches and show you some simple exercises to do at home.
- Leave any waterproof dressings on your knee until your post-operation review.
- You can put all your weight on your leg.
- You can put all your weight on your leg.
- Put ice on the knee for 20 minutes at a time, as frequently as possible.
- Post-operation review will usually be at 7-10 days.
- Physical therapy can begin after a few days or can be arranged at your first post-op visit.
- If you have any redness around the wound, increasing pain in the knee, have an elevated temperature or feel generally unwell, you should contact your surgeon as soon as possible.
Risks & Complications:
Complications are not common, but can occur. Prior to making the decision of having this operation, it is important you understand these so you can make an informed decision on the advantages and disadvantages of surgery.
Risks and complications can be Medical (Anesthesia) complications and surgical complications.
Medical (Anesthesia) Complications
Medical complications include those of the anesthetic and your general well being. Almost any medical condition can occur so this list is not complete. Complications include:
Allergic Reactions to Medications
- Blood loss requiring transfusion with its low risk of disease transmission.
- Heart attacks, strokes, kidney failure, pneumonia, and bladder infections.
- Complications from nerve blocks such as infection or nerve damage.
- Serious medical problems can lead to ongoing health concerns and prolonged hospitalization. The following is a list of surgical complications. These are all rare but can occur. Most are treatable and do not lead to long term problems.
Infection
Occurs approximately 1 in 200 cases. Treatment involves either oral or IV antibiotics, or rarely further surgery to wash the infection out.
Deep Vein Thrombosis
These are clots in the veins of the leg. If they occur you may need blood thinning medication in the form of injections or tablets. Very rarely they can travel to the lung (Pulmonary Embolus), which can cause breathing difficulties or even death.
Excessive Swelling & Bruising
This is due to bleeding in the soft tissues and will settle with time.
Joint stiffness
Can result from scar tissue within the joint, and is minimized by advances in surgical technique and rapid rehabilitation. Full range of movements cannot always be guaranteed.
Graft Failure
The graft can fail the same as a normal cruciate ligament does. Failure rate is approximately 5%. If the graft stretches or ruptures it can still be revised if required by using tendons from the other leg.
Damage to Nerves or Vessels
There are small nerves under the skin that cannot be avoided and cutting them can lead to areas of numbness in the leg. This normally reduces in size over time and does not cause any functional problems with the knee. Very rarely there can be damage to more important nerves or vessels causing weakness in the leg.
Hardware Problems
All grafts need to be fixed to the bone using various devices (hardware) such as screws or staples. These can cause irritation of the wound and may require removal once the graft has grown into the bone.
Donor Site Problems
Donor site is the location from where the graft is obtained. In general, either the hamstrings or patella tendon are used. There can be pain or swelling in these areas, which usually resolves over time.
Residual Pain
Can occur especially if there is damage to other structures inside the knee.
Reflex Sympathetic Dystrophy
This is an extremely rare condition that is not entirely understood, which can cause unexplained and excessive pain.
