Shoulder Arthroscopy
Shoulder arthroscopy is commonly used to diagnose and treat shoulder pain. It’s a type of keyhole surgery, which involves using a tiny camera to look inside your shoulder joint and repair any damage. It’s performed through small cuts in your skin.
You may be offered a shoulder arthroscopy if your shoulder has been damaged by an injury, arthritis or certain health conditions.
Preparing for shoulder Arthroscopy
Your surgeon will explain how to prepare for your procedure. If you smoke, for example, you will be asked to stop. Smoking increases your risk of getting a chest or wound infection, which can slow down your recovery. It can also make your surgery less effective and lead to complications.
Shoulder arthroscopy is usually done as a day-case procedure in a hospital. This means you have the procedure and go home on the same day.
You will usually have a shoulder arthroscopy under general anaesthesia. If you have a general anaesthetic, you’ll be asleep during the operation. Sometimes, your surgeon may use a combination of both local and general anaesthetics. Local anaesthesia completely stops you feeling any pain in your shoulder area. Occasionally, you may be able to have the whole operation under a local anaesthesia. This means you will stay awake during surgery. Your surgeon may offer you a sedative with the local anaesthetic. This relieves anxiety, makes you feel sleepy and helps you to relax during the operation.
If you're having a general anaesthetic, you’ll be asked to follow fasting instructions. This means not eating or drinking anything, usually for about six hours, before your surgery. It’s important to follow your anaesthetist’s advice.
You may be asked to wear compression stockings to help prevent blood clots forming in the veins in your legs. You may need to have an injection of an anticlotting medicine called heparin as well as, or instead of, wearing compression stockings.
Your nurse or surgeon will discuss with you what will happen before, during and after your procedure, including any pain you might have. If you’re unsure about anything, don’t be afraid to ask. No question is too small. It’s important that you feel fully informed so you feel happy to give your consent for the procedure to go ahead. You may be asked to do this by signing a consent form.
What are the alternatives to shoulder arthroscopy?
Not everyone who has a problem with their shoulder will need to have an arthroscopy. Your doctor will usually be able to diagnose your shoulder problem by examining you. You may also need to have some imaging tests, such as an X-ray, an ultrasound or an MRI scan.
The best treatment for your shoulder problem will depend on what’s caused the damage. Sometimes, your symptoms will improve on their own without treatment. Your doctor may suggest you try some self-help measures, such as doing exercises to strengthen the muscles around your shoulder. Other treatments for shoulder problems include physiotherapy and corticosteroid injections. Talk to your doctor about which treatment options are the right ones for you.
What happens during shoulder arthroscopy?
A shoulder arthroscopy often takes less than an hour. The length of your procedure will depend on how much work your surgeon needs to do inside your shoulder joint. You may have the surgery sitting in a deckchair position or lying on your side.
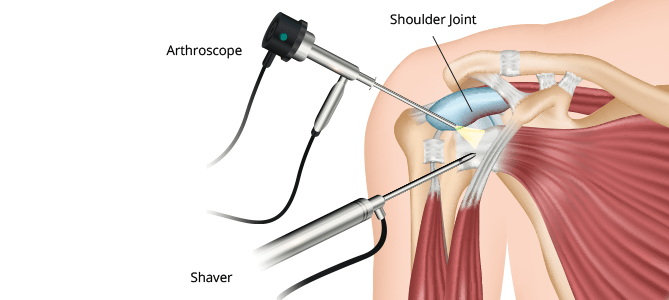
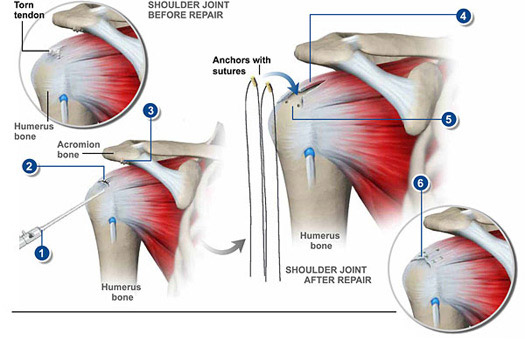
Once the anaesthetic has taken effect, your surgeon will make small cuts in the skin around your shoulder joint. They will then insert the arthroscope. This is like a tiny camera that your surgeon can use to view inside your shoulder joint.
Your surgeon will examine your shoulder joint by looking at images sent by the arthroscope to a monitor. If there’s any damage in your shoulder, they will insert surgical instruments to repair it. Your surgeon will also remove any damaged tissue that stops you moving your shoulder properly and causes pain.
Afterwards, your surgeon will close the cuts with stitches or adhesive strips. They will then wrap a dressing and a bandage around your shoulder.
It’s possible that your surgeon may need to change to open surgery during the procedure. This might be if they need to make a larger cut to repair a larger muscle tear. Your surgeon will talk to you about this risk before you consent to the procedure.
What to expect afterwards
You may need to rest until the effects of the anaesthetic have worn off. After a local anaesthetic, it may be several hours before the feeling comes back into your shoulder. Take special care not to bump or knock the area. You may have some discomfort as the anaesthetic wears off. You’ll be offered pain relief as you need it.
You will usually be able to go home when you feel ready. You'll need to arrange for someone to drive you home. Try to have a friend or relative stay with you for the first 24 hours after your shoulder arthroscopy.
Having a general anaesthesic or sedative affects everyone differently. You may find that you’re not so coordinated or that it’s difficult to think clearly. This should pass within 24 hours. In the meantime, don’t drive, drink alcohol, operate machinery or sign anything important. Always follow your surgeon’s advice.
Your nurse will give you some advice about caring for your healing wounds before you go home. You may be given a date for a follow-up appointment.
It will take a while for your dissolvable stitches to disappear. How long will depend on the type of stitches you have and how quickly your wound heals.
Your shoulder joint is likely to feel sore and stiff after surgery. Try to rest your arm. Applying a cold compress such as an ice pack or a bag of frozen peas wrapped in a towel may help to reduce swelling and bruising. But don’t apply ice directly to your bare shoulder as it can damage your skin.
Recovering from shoulder arthroscopy:
You may need to keep your arm in a sling after the operation. This will keep your shoulder in the right position to recover properly and will reduce any pain and swelling. The sling will also protect your shoulder from further damage until it’s fully recovered. Your surgeon will tell you how long you will need to wear a sling for.
You may struggle to dress and wash yourself at first – you may want to ask your partner, a relative or friend to be on hand to help you.. The first few weeks will be the most difficult – it should start to get easier after this.
If you need pain relief, you can take over-the-counter painkillers such as paracetamol or ibuprofen. Always read the patient information leaflet that comes with your medicine. If you have any questions, ask your pharmacist for advice.
Your physiotherapist will recommend some exercises for you. Doing these regularly will help your shoulder to heal and may help you to recover more quickly.
It usually takes several weeks to make a full recovery from shoulder arthroscopy. Most people get the full movement of their shoulder back afterwards, but this can take several months. Your recovery time will depend on what treatment if any, your surgeon performs on your shoulder joint. It will also make a difference how severe your shoulder problem is and how fit you are. It's important to follow your surgeon's advice.
You can usually drive once you’re fully mobile, but check with your doctor and motor insurance company first.
Side-effects of shoulder arthroscopy
After having a shoulder arthroscopy, you may get some unwanted side-effects, which are mostly temporary.
You may have small scars on your shoulder from the cuts made by your surgeon. Your shoulder and arm may be painful or uncomfortable for several weeks. You may also have some pain and stiffness around your shoulder.
Complications of shoulder arthroscopy
Complications are when problems occur during or after a procedure. The possible complications of any operation include an unexpected reaction to the anaesthetic, excessive bleeding or developing a blood clot, usually in a vein in your leg (called deep vein thrombosis, DVT).
Specific complications of arthroscopy include:
- Accidental damage to the inside of your joint
- An infection
- Excessive bleeding into your joint
- Damage to surrounding blood vessels or nerves
Remember – all medical procedures come with some risks. How these risks apply to you will be different from how they apply to others. Be sure to ask for more information if you have any concerns.
